Why place matters in health and social care
Most NHS and public health analysts already know that place matters. What is harder is answering the follow up questions that come in meetings: where exactly, how uneven, and what should we do about it.
Health and social care data is inherently spatial. Disease risk, deprivation, service access and outcomes all vary by geography. Yet much routine reporting still relies on tables and averages that smooth out local variation. This makes it easy to miss pockets of need and difficult to explain complex patterns clearly to decision makers.
Location intelligence adds practical context. By mapping health data, analysts can see patterns, inequalities and anomalies that are easy to overlook in tabular analysis, helping turn routine datasets into insight that supports real operational decisions.
Mapping disease incidence and health outcomes
Disease surveillance is a familiar task, but geography often changes how results are interpreted. A rate that looks stable at system level can mask sharp local variation.
Mapping disease incidence allows analysts to:
- Spot clusters or hotspots that have been averaged out in higher level reports
- Compare incidence and outcomes consistently across neighbourhoods or local authorities
- Track how patterns shift over time, supporting early warning and targeted response
For intelligence teams, maps also support faster sense checking. When questions arise about data quality or unexpected trends, a spatial view often highlights issues immediately, before deeper analysis is needed.
Understanding access to health services
Access to services is rarely just a numbers problem. Knowing how many GP practices or clinics exist says little about how easily people can reach them.
Healthcare access analysis benefits strongly from mapping, for example by:
- Visualising service locations alongside population density and need
- Exploring travel distance or drive time rather than straight line proximity
- Identifying areas where deprivation, growth or ageing populations are not matched by provision
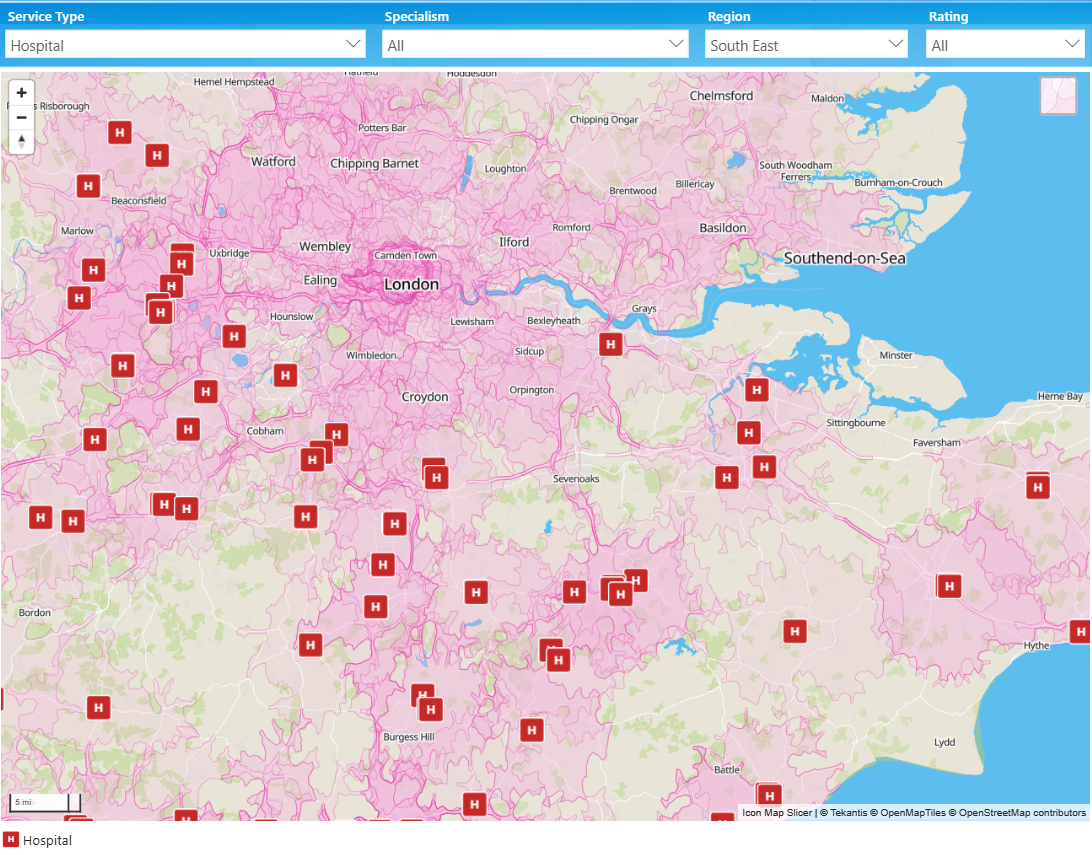
These insights support practical planning conversations around estate strategy, service redesign and community based care, grounding decisions in a shared, visual understanding of access. For example, the below image shows the 15 minute drivetime around each hospital.
Monitoring vaccination and screening coverage
Vaccination and screening programmes are often judged on overall uptake, but operationally the most important question is where coverage is lowest.
Vaccination coverage mapping helps analysts:
- Identify neighbourhoods with persistently lower uptake
- Compare patterns across cohorts, age groups or risk categories
- Monitor whether targeted interventions are improving coverage over time
This spatial view is particularly valuable during rollout phases, when teams need to prioritise outreach activity quickly and justify why certain areas are receiving additional focus.
Supporting operational planning and resource allocation
This is where location intelligence moves from analysis to influence. Analysts are regularly asked to support decisions such as:
- Where to locate temporary or mobile clinics
- Which communities to prioritise for outreach or visiting services
- How to deploy limited staff and resources most effectively
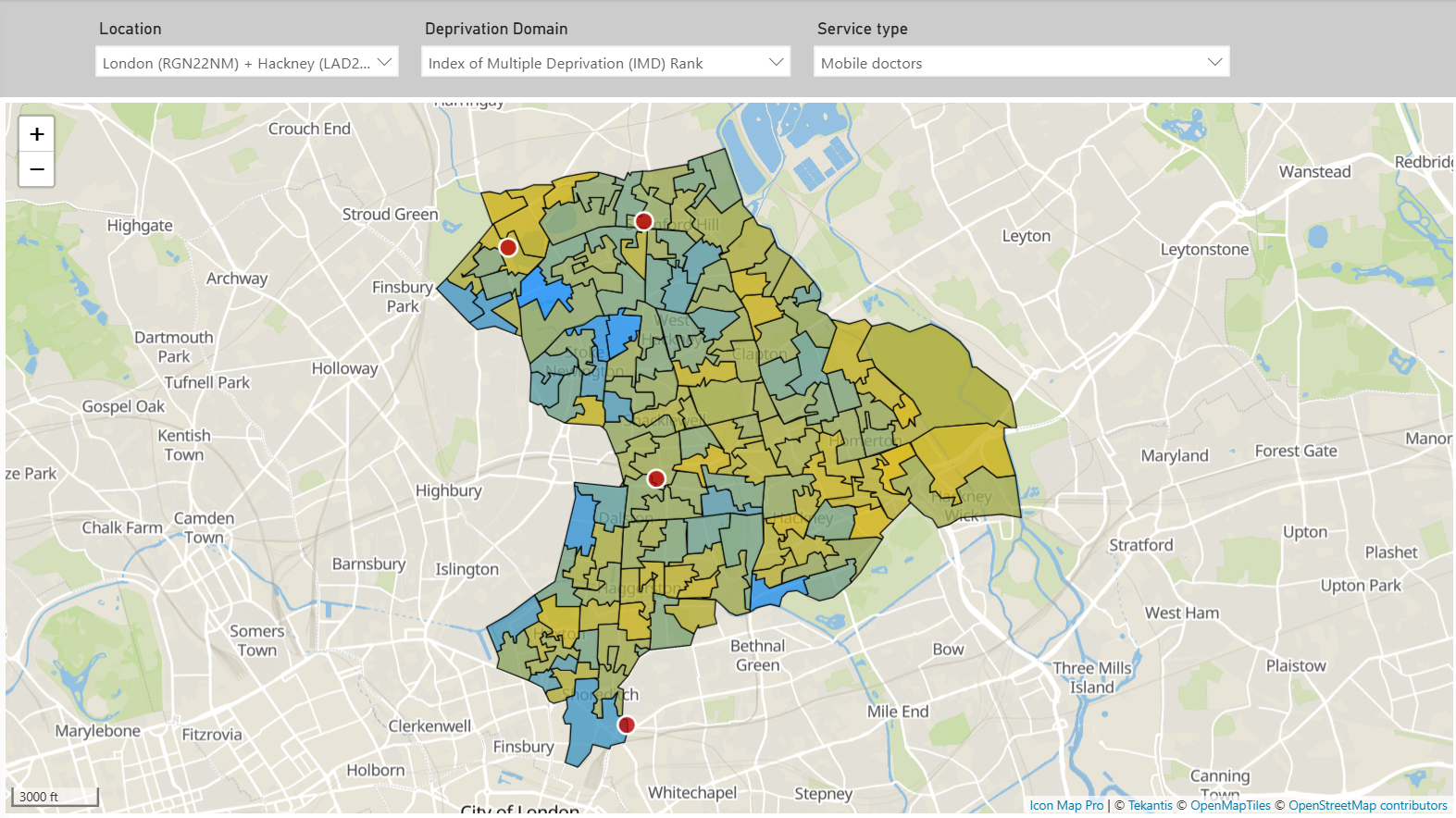
Maps help answer these questions by bringing multiple factors together, such as demand, capacity, workforce and access, into a single view. They also make trade offs easier to explain. A clear map often communicates risk and rationale more effectively than a set of charts or spreadsheets. For example, the below image shows the locations of mobile doctors and areas of deprivation within a London Borough.
Using modern analytics platforms for NHS mapping
For many NHS organisations, Power BI is already the primary environment for analysis and reporting. Embedding mapping within this platform keeps spatial insight close to trusted datasets and established governance.
This approach has practical benefits:
- Analysts work in familiar tools and workflows
- Maps refresh automatically as data updates
- Spatial insight becomes accessible to a wider audience, not just GIS specialists
Rather than introducing another system, location intelligence becomes an extension of everyday analytical practice.
Key takeaways for public health analysts
Location intelligence is not about producing more maps. It is about answering operational questions with greater clarity and confidence.
For NHS and public health analysts:
- Use maps where geography genuinely affects interpretation and decisions
- Focus on real planning questions, not just visualisation
- Treat spatial analysis as part of good analytical craft, not a specialist add on
When used well, mapping strengthens analysis, improves communication with decision makers, and supports more targeted, equitable health and care interventions.
If you want to explore how location intelligence can be applied within Power BI for public health analysis, consider looking at related examples or articles on mapping in public services.